When it comes to hospitals, so far in 2020 the biggest concern has been about them being totally overloaded due to the effects of the coronavirus pandemic. Images circulating online have shown exhausted medical staff, faces reddened and blotchy after long days wearing PPE masks and visors. Even without crises like the predicted shortage of ventilators in some places, most of us expect that hospital staff are busier than ever with patients right now.
It’s absolutely right to think that. Many of them are. But there are also scenarios in which medical professionals don’t have enough opportunity to ply their craft. One of those is training for surgical procedures.
Surgery residents have long been getting less hands-on experience than they would like. After completing residency, a large number say that they do not feel ready to perform core procedures independently. Since practice makes perfect, that’s not great news — and it could only be threatened further by coronavirus-induced social distancing, shuttering medical schools and causing many elective surgeries to be pushed back or put on hold.
Could virtual reality help?
Training the next generation
That’s the idea of Dr. Danny Goel, a surgeon based in Vancouver, BC, Canada. Goel is also the CEO and co-founder of a company called PrecisionOS, which makes VR surgical training tools for those who need them. They can be used for upskilling existing surgeons or allowing them to maintain their high level of skill. Alternatively they can help train the next generation of surgeons and medical professionals so that they’re ready — and practiced — to save lives when the time comes.

“Outside of direct patient care, a current solution has yet to be implemented for low risk, yet highly impactful and efficient [education of] surgeons, trainees, and other health care providers on a global scale,” Goel told Digital Trends. “The current models are limited in access and utility. Virtual reality training and education permits the end-user to make decisions while realizing the impact of those decisions. This will serve as a tool for assessment and provides greater insight on how we may improve as a global medical community.”
PrecisionOS wasn’t developed with the current coronavirus pandemic in mind. Unless you’re a company founded in the past few months, no business imagined the way that COVID-19 would change the habits and way of life of large quantities of people. But it nonetheless reflects a change that has only been becoming more prominent in recent years.
The idea was to find a way to allow trainees to practice procedures over and over without exposing patients to risk. Cadavers are an alternative for this kind of training, although they are frequently in short supply — and, when they are available, can only be practiced on in certain contexts.
The VR-tuous circle of value
Previous studies have shown that the highest volume surgeries typically yield the best outcomes for patients. Low volume surgeries, by comparison, can mean increased complications, longer periods of time spent in the operating room, and higher costs. This is sometimes referred to as the “virtuous circle of value,” whereby greater patient volume and, therefore, practice means more rapidly accumulated experience, which translates into better results.
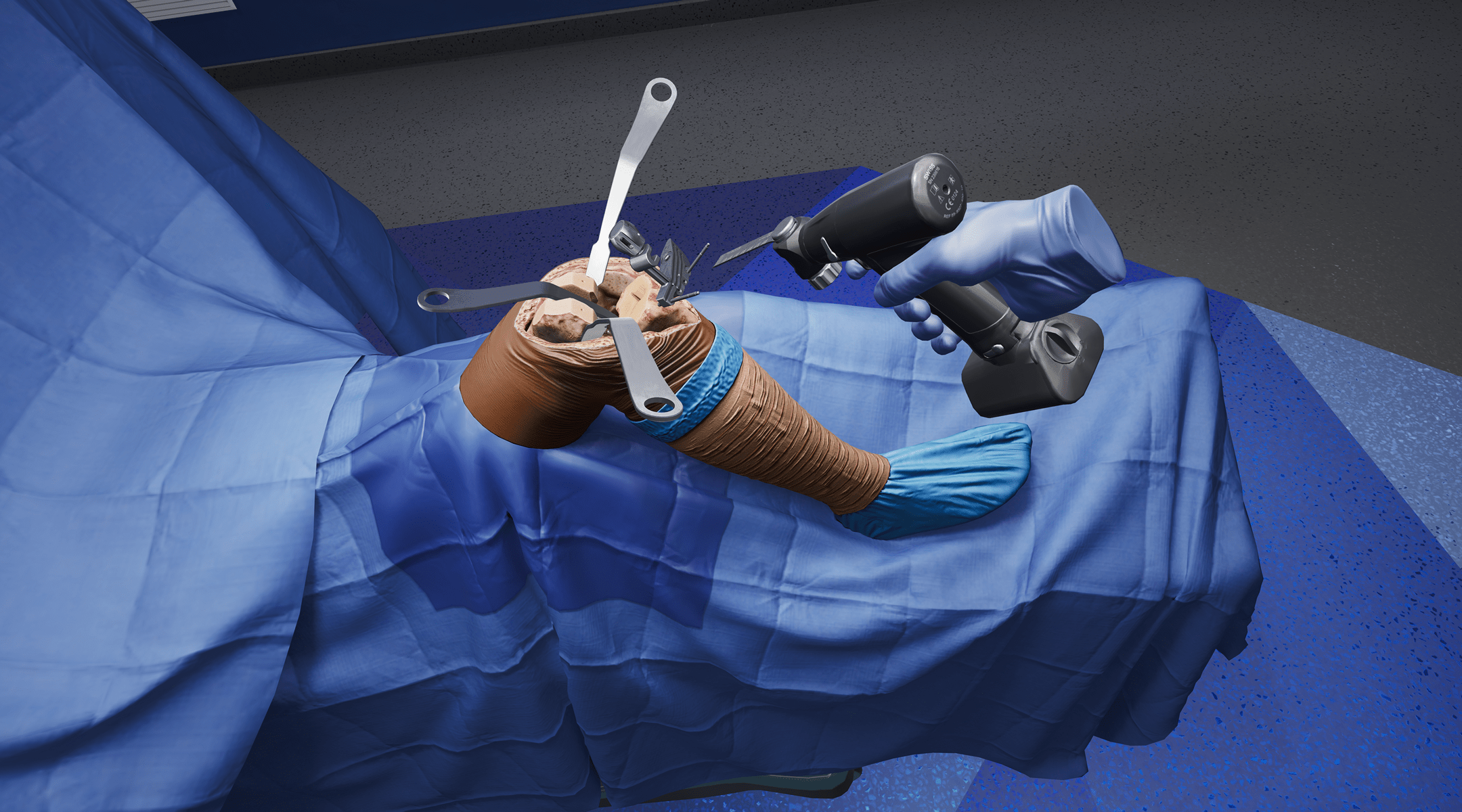
A gamified virtual reality system like the one that PrecisionOS has developed poses one high-tech answer. “All surgical procedures can be simulated [with our software],” Goel said. “The only hardware that is required is a standalone and untethered headset. Currently we are using the Oculus Quest. All the information is available on this hardware, which can be used anywhere at any time.”

The procedures themselves are carried out using generic VR controllers. While that might not be perfect for fine-grain practice (other VR training systems include specialist controllers, although they can only simulate a limited number of procedures as a result), it’s still enough for people to get to grips with particular operations.
PrecisionOS’s VR setup allows users to both get some one-on-one practice carrying out procedures, as well as working together in a group, via a multiplayer feature. This enables various avatars to carry out virtual sessions together — even when “together” might mean in entirely different locations.
“In my opinion, this technology is a major disruption of education and learning in surgery,” Goel said. “We are not digitizing our current model of training, but are challenging it through layers of depth and complexity.”
The PrecisionOS system is already being used by several training programs and institutions. Goel said that the “most integrated” use of the technology has been at the University of Connecticut, which has been using the system for the past few months. “We have since rolled out to many others, including the Mayo Clinic,” Goel said.
The future of medicine is here
Incorporating emerging technologies into medicine poses a challenge. Reasons for this can range from the complexities of FDA regulation to the high human cost of getting something wrong. The Silicon Valley mantra of “move fast, break things” understandably works a lot better for A/B testing of new user interface elements than it does A/B testing of new ways to treat yourself or your loved ones.

Nonetheless, there have been some impressive advances in recent years, driven by breakthroughs in technology. Smart surgical glasses bring augmented reality into the operating room. HD endoscopes allow surgeons to look around inside patients without having to make large incisions. And, befitting the age of social distancing, 5G and advanced surgical telerobots make it possible for operations to be carried out without the lead surgeon having to be in the room — or even the same state — as the patient.
Isn’t it about time that medical training took the same leap into the future?


